
What do I need to
know about my first visit?
When first visiting Dr. Gianfortune it is very important to bring your
insurance card, a list of your current medications and if you are under the age
of 18 you must have a parent present during treatment.
If you have a history of heart disease or hip replacement contact your
medical physician regarding the need for pre-medication of antibiotics prior to
your visit with Dr. Gianfortune. The American Heart Association recommends
pre-medication with antibiotic in some conditions, this prescription should come
form your medical physician.
What Is A Dental
Emergency?
Injuries to the mouth may include teeth that are knocked out (avulsed),
forced out of position and loosened (extruded) or fractured. In addition, lips,
gums or cheeks are often cut. Oral injuries are often painful and should be
treated by Dr. Gianfortune as soon as possible.
How
soon should I see a dentist?
Immediately. Getting to a dentist with 30 minutes can make the difference
between saving or losing a tooth.
When a tooth is knocked out:
-
Immediately call your dentist
for an emergency appointment.
-
Handle the tooth by the crown,
not the root. Touching the root (the part of the tooth below the gum) can
damage cells necessary for bone re-attachment.
-
Gently rinse the tooth in
water to remove dirt. Do not scrub.
-
Place the clean tooth in your
mouth between the cheek and gum to keep it moist. It is important not to let
the tooth dry out.
-
If it is not possible to store
the tooth in the mouth of the injured person, wrap the tooth in a clean
cloth or gauze and immerse in milk.
When a tooth is pushed out of position:
-
Attempt to reposition the
tooth to its normal alignment using very light finger pressure, but do not
force the tooth.
-
Bite down to keep the tooth
from moving.
-
Dr. Gianfortune may splint the
tooth in place to the two healthy teeth next to the loose tooth.
What Is A Denture?
A denture is a removable replacement for missing teeth and adjacent tissues.
It is made of acrylic resin, sometimes in combination with various metals.
Complete dentures replace all the teeth, while a partial denture fills in the
spaces created by missing teeth and prevents other teeth from changing position.
Complete dentures are either "conventional" or "immediate." A conventional
denture is placed in the mouth about a month after all the teeth are removed to
allow for proper healing, whereas an immediate denture is placed as soon as the
teeth are removed. The drawback with an immediate denture is that it may require
more adjustments after the healing has taken place.
Who
needs a denture?
Candidates for complete dentures have lost most or all of their teeth. A
partial denture is suitable for those who have some natural teeth remaining. A
denture improves chewing ability and speech, and provides support for facial
muscles. It will greatly enhance the facial appearance and smile.
What happens when you get a denture?
Dr. Gianfortune can make a full conventional denture when all teeth have been
lost or all extraction sites have healed (up to eight weeks or longer.) The
denture process takes about one month and five appointments: the initial
diagnosis is made; an impression and a wax bite are made to determine vertical
dimensions and proper jaw position; a "try-in" is placed to assure proper color,
shape and fit; and the patient's final denture is placed, following any minor
adjustments.
New denture wearers need time to get accustomed to their new "teeth" because
even the best fitting dentures will feel awkward at first. While most patients
can begin to speak normally within a few hours, many patients report discomfort
with eating for several days to a few weeks. To get accustomed to chewing with a
new denture, start with soft, easy-to-chew foods. In addition, denture wearers
often notice a slight change in facial appearance, increased salivary flow, or
minor speech difficulty.
How
do you care for a denture?
A denture is fragile, so it is important to handle it with care. Remove and
brush the denture daily, preferably with a brush designed specifically for
cleaning dentures, using either a denture cleanser or toothpastes. Never use
harsh, abrasive cleansers, including abrasives toothpastes, because they may
scratch the surface of the denture. Don't sterilize your denture with boiling
water because it will cause it to become warped. If you wear a partial denture
be sure to remove it before brushing your natural teeth.
When not in use, soak it in a cleanser solution or in water. Get in the habit
of keeping the denture in the same safe and handy place to reduce the likelihood
of misplacement.
Should a denture be worn at night?
While you may be advised to wear your denture almost constantly during the
first two weeks- even while you sleep-under normal circumstances it is
considered best to remove it at night. Research has shown that removing the
denture for at least eight hours during either the day or night allows the gum
tissue to rest and allows normal stimulation and cleansing by the tongue and
saliva. This promotes better long-term health of the gums.
Continue seeing Dr. Gianfortune regularly.
It is important to continue having regular dental checkups so that
Dr.Gianfortune can examine oral tissues for signs of disease. As of aging, your
mouth will continue to change as the bone under your denture shrinks or recedes.
To maintain a proper fit over time, it may be necessary to reline (resurface the
inside) your denture to insure a proper fit. Never attempt to adjust a denture
yourself and do not use denture adhesives for a prolonged period because it can
contribute to bone loss. When in doubt, consult Dr.Gianfortune.
Are
there any alternatives to dentures?
Dentures are no longer the only way to restore a mouth that has few teeth.
Strategically placed support, or implants, can now be used to support
permanently cemented bridges, or anchors for a partial denture. The cost tends
to be greater, but the implants and bridges more closely resemble the "feel" of
real teeth. Dental implants are becoming the alternative of choice to dentures,
but not everyone is a candidate for implants. Consult Dr. Gianfortune for
advice.
How Can I Take
Care Of My Teeth?
Proper oral care can keep you smiling well into retirement. Brushing at least
twice a day with a fluoride toothpaste and a soft-bristle brush are as important
as ever. Flossing can help you save your teeth by removing plaque between teeth
and below the gum line that your toothbrush cannot reach.
What are some problems I should watch for?
Gingivitis. Most people don't realize how important it is to take care of
their gums. Gingivitis is caused by the bacteria found in plaque that attack the
gums. Symptoms of gingivitis include red, swollen gums and possible bleeding
when you brush. If you have any of these symptoms, see Dr. Gianfortune at once.
Gingivitis can lead to gum disease if problems persist. Three out of four adults
over age 35 are affected by some sort of gum (periodontal) disease. In gum
disease, the infection becomes severe. Your gums begin to recede, pulling back
from the teeth. In the worst cases, bacteria form pockets between the teeth and
gums, weakening the bone. All this can lead to tooth loss if untreated,
especially in patients with osteoporosis. If regular oral care is too difficult,
Dr.Gianfortune can provide alternatives to aid in flossing and prescribe
medication to keep the infection from getting worse.
What if it's too difficult to brush?

If you have arthritis, you may find it difficult to brush and floss for good
oral health care and prevention of disease. Ask Dr. Gianfortune for ways to
overcome this problem. Certain dental products are designed to make dental care
less painful for arthritis sufferers. You may want to try strapping the
toothbrush to a larger object, such as a ball, to make the brush more
comfortable to handle, or electric toothbrushes can help by doing some of the
work for you.
Should I be concerned about dry mouth?
Dry mouth (xerostomia) happens when salivary glands fail to work due to
disease, certain medications or cancer treatment. This can make it hard to eat,
swallow, taste and speak. In certain cases, such as radiation therapy, dry mouth
can lead to severe complications, which is why it is important you see Dr.
Gianfortune immediately before beginning any form of cancer treatment. Drinking
lots of water and avoiding sweets, tobacco, alcohol and caffeine are some ways
to fight dry mouth.
Periodontal Disease
Diagnosis
Periodontal disease is diagnosed by your dentist or dental hygienist during a
periodontal examination.
This type of exam should always be part of your regular dental
check-up.
A periodontal probe (small dental instrument) is gently used to measure the
sulcus (pocket or space) between the tooth and the gums. The depth of a healthy
sulcus measures three millimeters or less and does not bleed. The periodontal
probe helps indicate if pockets are deeper than three millimeters. As
periodontal disease progresses, the pockets usually get deeper.
Your dentist or hygienist will use pocket depths, amount of bleeding,
inflammation, tooth mobility, etc., to make a diagnosis that will fall into a
category below:
Gingivitis
Gingivitis is the first stage of periodontal disease. Plaque and its toxin
by-products irritate the gums, making them tender, inflamed, and likely to
bleed.
Periodontitis
Plaque hardens into calculus (tartar). As calculus and plaque continue to
build up, the gums begin to recede from the teeth. Deeper pockets form between
the gums and teeth and become filled with bacteria and pus. The gums become
very irritated, inflamed, and bleed easily. Slight to moderate bone loss may be
present.
Advanced
Periodontitis
The teeth lose more support as the gums, bone, and periodontal ligament
continue to be destroyed. Unless treated, the affected teeth will become very
loose and may be lost. Generalized moderate to severe bone loss may be present.
Treatment
Periodontal treatment methods depend upon the type and severity of the
disease. Your dentist and dental hygienist will evaluate for periodontal
disease and recommend the appropriate treatment.
Periodontal disease progresses as the sulcus (pocket or space) between the
tooth and gums gets filled with bacteria, plaque, and tartar, causing irritation
to the surrounding tissues. When these irritants remain in the pocket space,
they can cause damage to the gums and eventually, the bone that supports the
teeth!
If the disease is caught in the early stages of
gingivitis, and no damage has been done,
one to two regular cleanings will be recommended. You will also be given
instructions on improving your daily oral hygiene habits and having regular
dental cleanings.
If the disease has progressed to more advanced stages, a special periodontal
cleaning called
scaling and root planning
(deep cleaning)
will be recommended. It is usually done one quadrant of the mouth at a time
while the area is numb. In this procedure, tartar, plaque, and toxins are
removed from above and below the gum line (scaling)
and rough spots on root surfaces are made smooth (planning). This procedure helps gum
tissue to heal and pockets to shrink. Medications, special medicated mouth
rinses, and an electric tooth brush may be recommended to help control infection
and healing.
If the pockets do not heal after scaling and root planning, periodontal
surgery may be needed to reduce pocket depths, making teeth easier to clean.
Your dentist may also recommend that you see a Periodontist (specialist of the
gums and supporting bone).
Maintaining your overall health
Studies have shown that maintaining a healthy mouth may keep your body
healthier and help you avoid diabetes, heart disease and stroke. The best way to
achieve good oral health is to visit Dr. Gianfortune for a cleaning at least
twice a year.
|
Root Canal Treatment |
|
|
|
If your tooth's nerve chamber becomes infected by decay,
root canal treatment is often the only way to save your tooth. |
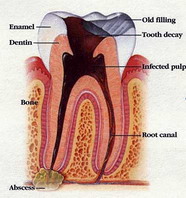
|
|
|
Inside your tooth's hard outer shell is a nourishing pulp of
blood vessels, lymph vessels, and nerves. The root canals, which contain
the pulp, extend to the bone. Deep tooth decay, or an injury, can cause
serious damage and infection to the pulp's nerves and vessels. Root
canal, or endodontic, treatment cleans out the infected pulp chamber ad
repairs the damage.
Some indications of the need for root canal treatment may be:
-
Spontaneous pain or throbbing while biting.
-
Sensitivity to hot and cold foods.
-
Severe decay or an injury that creates an abscess (infection) in the
bone.
|
The Procedure |
|
|
|
 |
 |
 |
|
Step 1 |
Step 2
|
Step 3 |
|
After the tooth is anesthetized, an opening
is made through the crown into the pulp chamber.
|
The length of the root canals is determined |
Unhealthy pulp is removed. Canals are cleaned, enlarged
and shaped. |
|
|
 |
 |
|
Step 4
|
Step 5 |
|
Canals are filled and sealed. A metal
post may be added for structural support
or to retain restorative materials. |
The tooth is sealed with a temporary filling. Usually a
gold or porcelain crown adds further protection. |
|
|
|
|
The material used to fill your root canal will probably last
you a lifetime, but eventually the filling or crown may need to
be replaced. |
|
|
|
Be sure to
follow the special home care instructions provided by Dr.
Gianfortune.
|
Wisdom Teeth |
|
|
|
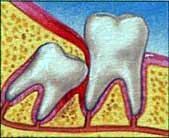
Wisdom teeth, or third molars, are the final teeth to
develop. Most of us have four wisdom teeth, one in
each corner of the mouth. They usually emerge during
our late teens or early twenties. Often wisdom teeth
become trapped, or impacted, in the jawbone and
cause crowding, displacement, decay, infection, or
gum disease. Impacted wisdom teeth can grow in many
different directions: horizontally, vertically, or
at an angle. |
|
|
|
 |
 |
|
Angular, bony impaction of third molar
(wisdom tooth). |
Soft tissue impaction of third molar
(wisdom tooth). |
|
|
|
|
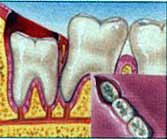
In most cases, it is recommended that impacted wisdom teeth
are extracted. Wisdom tooth surgery is performed,
usually under local anesthesia, in your dentist's
office, an outpatient surgical facility, or a
hospital. Make arrangements for a responsible adult
to drive you home and plan to rest at home for the
remainder of the day. |
|
|
|
The Procedure |
|
|
|
 |
|
 |
|
Incision is made and overlying bone is
removed, exposing crown of impacted tooth
|
|
Tooth is extracted whole or surgically
sectioned. The site is sutured closed.
|
|
|
|
|
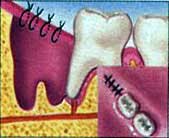
To ease any discomfort and promote healing:
-
Use ice packs on the cheek for swelling,
alternating on and off every thirty minutes.
-
Apply biting pressure with clean gauze to stop
bleeding.
-
Eat soft foods and drink extra liquids.
-
Avoid hard or crunchy foods in the tender area.
-
Brush carefully the day after surgery.
-
Take prescribed medications and follow all
instructions as directed.
Call your doctor immediately in case of excessive bleeding
or swelling, persistent, severe pain or fever.
|
|
|
Why Are My Teeth
Sensitive?
Tooth sensitivity is caused by the stimulation of cells within tiny tubes
located in the dentin (the layer of tissue found beneath the hard enamel that
contains the inner pulp). When the hard enamel is worn down or gums have
receded-causing the tiny tube surfaces to be exposed-pain can be caused by
eating or drinking food and beverages that are hot or cold; touching your teeth;
or exposing them to cold air. Hot and cold temperature changes cause your teeth
to expand and contract. Over time, your teeth can develop microscopic cracks
that allow these sensations to seep through to the nerves. Exposed areas of the
tooth can cause pain and even affect or change your eating, drinking and
breathing habits. Taking a spoonful of ice cream, for example, can be a painful
experience for people with sensitive teeth.
Is
tooth sensitivity a common condition?
Sensitive teeth is one of the most common complaints among dental patients.
At least 45 million adults in the United States and 5 million Canadians, suffer
at some time from sensitive teeth.
What can I do about sensitive teeth?
Tooth sensitivity can be reduced by using a desensitizing toothpaste,
applying sealants and other desensitizing ionization and filling materials
including fluoride by your dentist, and decreasing the intake of acid-containing
foods. Tartar control toothpastes will sometimes cause teeth to be sensitive as
well as drinking diet soft drinks throughout the day.
Avoid using hard bristled toothbrushes and brushing your teeth too hard,
which can wear down the tooth's root surface and expose sensitive spots. The way
to find out if you're brushing your teeth too hard is to take a good look at
your toothbrush. If the bristles are pointing in multiple directions, you're
brushing too hard.
What can the dentist do for my sensitive teeth?
Dentists have a variety of regimens to manage tooth hypersensitivity,
including both in-office treatments and patient-applied products for home use.
If you are diagnosed with dentin hypersensitivity, your dentist may apply a
desensitizing agent or a protective coating. You may be prescribed a stannous
fluoride gel or an over-the-counter desensitizing toothpaste containing fluoride
and either potassium nitrate or strontium chloride. These ingredients help block
transmission of sensation from the tooth to the nerve. It also might help to
massage the special paste onto your gums with your finger after brushing.
Why Do I Need
X-rays?
Radiographic or X-ray examinations provide Dr.Gianfortune with an important tool
that shows the condition of your teeth, its roots, jaw placement and the overall
composition of your facial bones. X-rays can help Dr. Gianfortune determine the
presence or degree of periodontal disease, abscesses and many abnormal growths,
such as cysts and tumors. X-rays also can show the exact location of impacted
and unerupted teeth. They can pinpoint the location of cavities and other signs
of disease that may not be possible to detect through a visual examination.
Do
all patients have X-rays taken every six months?

No. Your radiographic schedule is based on Dr. Gianfortune's assessment of
your individual needs, including whether you're a new patient or a follow-up
patient, adult or child. In some cases, new patients require a full set of mouth
X-rays to evaluate oral health status, including any underlying signs of gum
disease and for future comparison. Follow-up patients may require X-rays to
monitor their gum condition or their chance of tooth decay.
Should
I be concerned about exposure to radiation?
All health care providers are sensitive to patients' concerns about exposure
to radiation. Dr.Gianfortune has been trained to prescribe radiographs when they
are appropriate and to tailor radiographic schedules to each patient's
individual needs. By using state-of-the-art technology and by staying
knowledgeable about recent advances, Dr. Gianfortune knows which techniques,
procedures and X-ray films can minimize your exposure to radiation
What is orofacial pain?
| Orofacial pain includes
a number of clinical problems involving the chewing (masticatory)
muscles or temporomandibular joint. Problems can include
temporomandibular joint discomfort; muscle spasms in the head, neck and
jaw; migraines, cluster or frequent headaches; pain with the teeth, face
or jaw; or anxiety or depression You swallow approximately 2,000 times
per day, which causes the upper and lower teeth to come together and
push against the skull. People who have an unstable bite, missing teeth,
or poorly aligned teeth can have trouble because the muscles work harder
to bring the teeth together, causing strain. Pain also can be caused by
clenching or grinding teeth, trauma to the head and neck, or poor
ergonomics.
Some may experience pain in the ears, eyes, sinuses, cheeks or side
of the head, while others experience clicking when moving the jaw or
even locking if the jaw is opened or closed.
Temporomandibular disorders (TMD) also
known as TMJ
The National Institutes of Health estimates that more than 10 million
Americans have TMD, or problems affecting the jaw joint and/or muscles.
Your temporomandibular joints are located where the skull connects to
your lower jaw. To feel these joints, place your fingers in front of
both ears and open your mouth. The muscles on the sides of your head and
face control the joints' movements. Researchers believe women between 20
and 40 are most likely to suffer from TMD because of the added estrogen
in their bodies.
Headaches
One in eight Americans suffers from headaches. Experts estimate that
80 percent of all headaches are caused by muscle tension, which may be
related to the bite. Headaches also can be caused by clenching jaw
muscles for long periods of time. Signs that may indicate a headache
from a dental origin include:
-
Pain behind the eyes
-
Sore jaw muscles or "tired" muscles upon awaking
-
Teeth grinding
-
Clicking or popping jaw joints
-
Head and/or scalp is painful to the touch
-
Earaches or ringing
-
Neck, shoulder or back pain
-
Dizziness
-
Sleep disorders
If you have gone through treatment and still experience orofacial
pain, you may have a sleep disorder, such as bruxism, or a sleep-related
breathing disorder, such as snoring or sleep apnea. Bruxism is the
technical term for grinding and clenching. Snoring that goes undiagnosed
may lead to an increased tendency for the airway to collapse, leading to
sleep apnea. Sleep apnea is a condition when the tissues and muscles in
the back of the throat collapse the airway. This can cause a person to
wake up multiple times in the middle of the night, sometimes without
knowing it.
Are there any treatments available?
Dr. Gianfortune has a variety of treatments that will help alleviate
your orofacial symptoms. One device is called an orthotic, or splint,
that is worn over the teeth until the bite can be stabilized. Permanent
correction may require reshaping teeth, building crowns, orthodontics,
or a permanent appliance for the mouth.
Other ways to alleviate the pain include:
-
Place an ice pack on the painful area for 10 minutes, three or four
times per day.
-
Eat softer foods and avoid chewing gum or ice.
-
Cut food into smaller pieces.
-
Keep upper and lower teeth slightly apart except when chewing or
swallowing. Keeping your tongue between your teeth may help with
this.
-
Sleep on your back.
-
Don't rest your hand on your chin. When talking on the phone don't
rest the receiver on your shoulder.
|
When should my child first
see a dentist, and why?

The ideal
time is around 3 years old, unless you suspect a problem. This time frame is a
perfect opportunity for the dentist to carefully examine the development of your
child's mouth. Because dental problems often start early, the sooner the visit
the better. To safeguard against problems such as baby bottle tooth decay,
teething irritations, gum disease, and prolonged thumb-sucking, Dr. Gianfortune
can provide or recommend special preventive care.
What will happen on my child's first visit?
Many first visits are nothing more than introductory icebreakers to acquaint
your child with the hygienist, Dr. Gianfortune and the practice. If the child is
frightened, uncomfortable or non-cooperative, a referral to a pediatric dentist
may be necessary. Patience and calm on the part of the parent and reassuring
communication with your child are very important in these instances.
If the child is compliant, the first session often lasts between 15-30
minutes and may include the following, depending on age:
A gentle but thorough examination of the teeth, jaw, bite, gums and oral
tissues to monitor growth and development and observe any problem areas; If
indicated, a gentle cleaning, which includes polishing teeth and removing any
plaque, tartar build-up and stains.
-
Dr. Gianfortune and his staff
will be able to answer any questions you have and try to make you and your
child feel comfortable throughout the visit. The entire dental team and the
office will provide a relaxed, non- threatening environment for your child.
Five ways to protect your child's oral health at home:
Parents typically provide oral hygiene care until the child is old enough to
take personal responsibility for the daily dental health routine of brushing and
flossing. A proper regimen of preventive home care is important from the day
your child is born.
-
Clean your infant's gums with
a clean, damp cloth.
-
As soon as the first teeth
come in, begin brushing them with a small, soft-bristled toothbrush and a
pea-sized dab of fluoride toothpaste. Remember, most children are also
getting fluoride from the community water supply.
-
To avoid baby bottle tooth
decay and teeth misalignment due to sucking, try to wean your child off of
the breast and bottle by one year of age, and monitor excessive sucking of
pacifiers, fingers and thumbs. Never give your child a bottle of milk, juice
or sweetened liquid as a pacifier at naptime or bedtime. Help a young child
brush at night-the most important time to brush, due to lower salivary flow
and higher susceptibility to cavities and plaque. Perhaps let the child
brush their teeth first to build self-confidence, then the parent can follow
up to ensure that all plaque is removed. Usually by age 5 or so, the child
can learn to brush his or her own teeth with proper parental instruction.
-
The best way to teach a child
how to brush is to lead by good example. Allowing your child to watch you
brush your teeth teaches the importance of good oral hygiene.
Back to Top
|
|



